A mysterious flu-like illness has emerged in the Democratic Republic of Congo (DRC), causing significant concern just months after the mpox emergency declaration. The outbreak, centered in the remote Panzi health zone of Kwango province, has claimed the lives of over 70 people, predominantly children under 14, since October. Denise Kabeya, a resident of Panzi, tragically lost her 12-year-old daughter to the disease after initially mistaking the symptoms for malaria or typhoid fever – common ailments in the region. The rapid progression of the illness and the subsequent deaths have left communities fearful and demanding answers.
Between October and mid-December, over 500 cases of the undiagnosed illness were reported within the Panzi health zone. The World Health Organization (WHO), in collaboration with Congolese health authorities, has dispatched experts to investigate the outbreak and assist with the response. While laboratory tests have revealed the presence of malaria in some samples, the exact cause of the illness remains elusive. The WHO Director-General acknowledged the possibility of multiple diseases contributing to the outbreak’s severity. The remote location of Panzi, coupled with limited infrastructure and testing capacity, has hampered efforts to identify and combat the disease.
Symptoms of the illness resemble those of the flu, including high fever, headaches, coughing, runny nose, and body aches. Some children have also experienced respiratory distress and anemia, which have contributed to fatalities. Furthermore, underlying malnutrition has exacerbated the disease’s impact on some children. The lack of essential medical equipment, like oxygen condensers and isolation facilities, along with the absence of electricity and reliable communication, have severely constrained the ability of healthcare workers to effectively treat patients in the Panzi hospital.
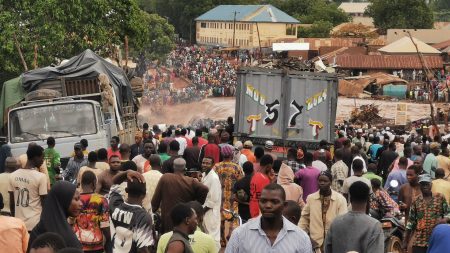
The geographical isolation of Panzi, situated approximately 700km from the capital Kinshasa, has posed significant logistical challenges. Poor road conditions, particularly during the rainy season, have hampered access to the affected area, delaying the deployment of medical teams and the transportation of laboratory samples. Samples collected in Panzi must be transported over 500km to Kikwit for testing, further hindering the diagnostic process. This delay in identifying the root cause of the outbreak has exacerbated the crisis. The WHO, while acknowledging these challenges, has affirmed its commitment to supporting patient treatment, risk communication, and community engagement.
As the outbreak continues, concerns are mounting about its potential spread to neighboring communities. Residents outside of Panzi are expressing anxiety over the perceived lack of preventative measures by provincial authorities. Calls for enhanced epidemiological surveillance, temperature checks, and hand-washing stations along main roads leading to the affected zone are growing louder. One local health expert, speaking anonymously, voiced concerns about a possible zoonotic origin of the disease, suggesting a link between contact with wild animals and the onset of illness. Although no official confirmation of an animal connection has been made, the expert advised caution in interactions with wildlife.
This new health crisis unfolds against a backdrop of existing health challenges in the Panzi region. Typhoid fever, measles, and high levels of malnutrition, coupled with low vaccination rates, render children particularly vulnerable. The current outbreak has strained local health facilities already grappling with these pre-existing burdens. Dr. Rufin Mukuwa, a physician at the Panzi general referral hospital, described treating 15 to 20 patients daily, noting similarities between some symptoms and those of COVID-19. In the absence of a definitive diagnosis, medical staff are providing symptomatic treatment, including antibiotics for respiratory complications and paracetamol for pain relief. While this approach provides some respite, the underlying cause of the illness remains unknown, adding to the urgency of the ongoing investigation. The outbreak also coincides with an ongoing mpox epidemic in the DRC, further stretching the country’s healthcare resources and underscoring the urgent need for a comprehensive response to address these converging health crises.