Mosquitoes, notorious vectors of diseases like malaria, dengue fever, and yellow fever, may surprisingly hold the key to combating one of their own deadliest payloads. Researchers in the Netherlands have pioneered a novel approach to malaria vaccination, utilizing genetically modified mosquitoes as vaccine delivery systems. This innovative strategy aims to harness the mosquito’s natural transmission mechanism to elicit a robust immune response against the malaria parasite, specifically Plasmodium falciparum, the deadliest of the malaria-causing parasites.
The core principle of this "flying vaccinator" approach involves genetically weakening the P. falciparum parasite. By removing a crucial gene, scientists have engineered a parasite strain capable of infecting humans but incapable of causing full-blown malaria. This modified parasite, when delivered via a mosquito bite, initiates an infection within the liver, the parasite’s initial replication site. However, due to the missing gene, the parasite’s life cycle is interrupted, preventing it from progressing to the bloodstream and causing debilitating symptoms. This localized liver-stage infection, while harmless, triggers a potent immune response, effectively priming the body to fight off future encounters with the actual malaria parasite.
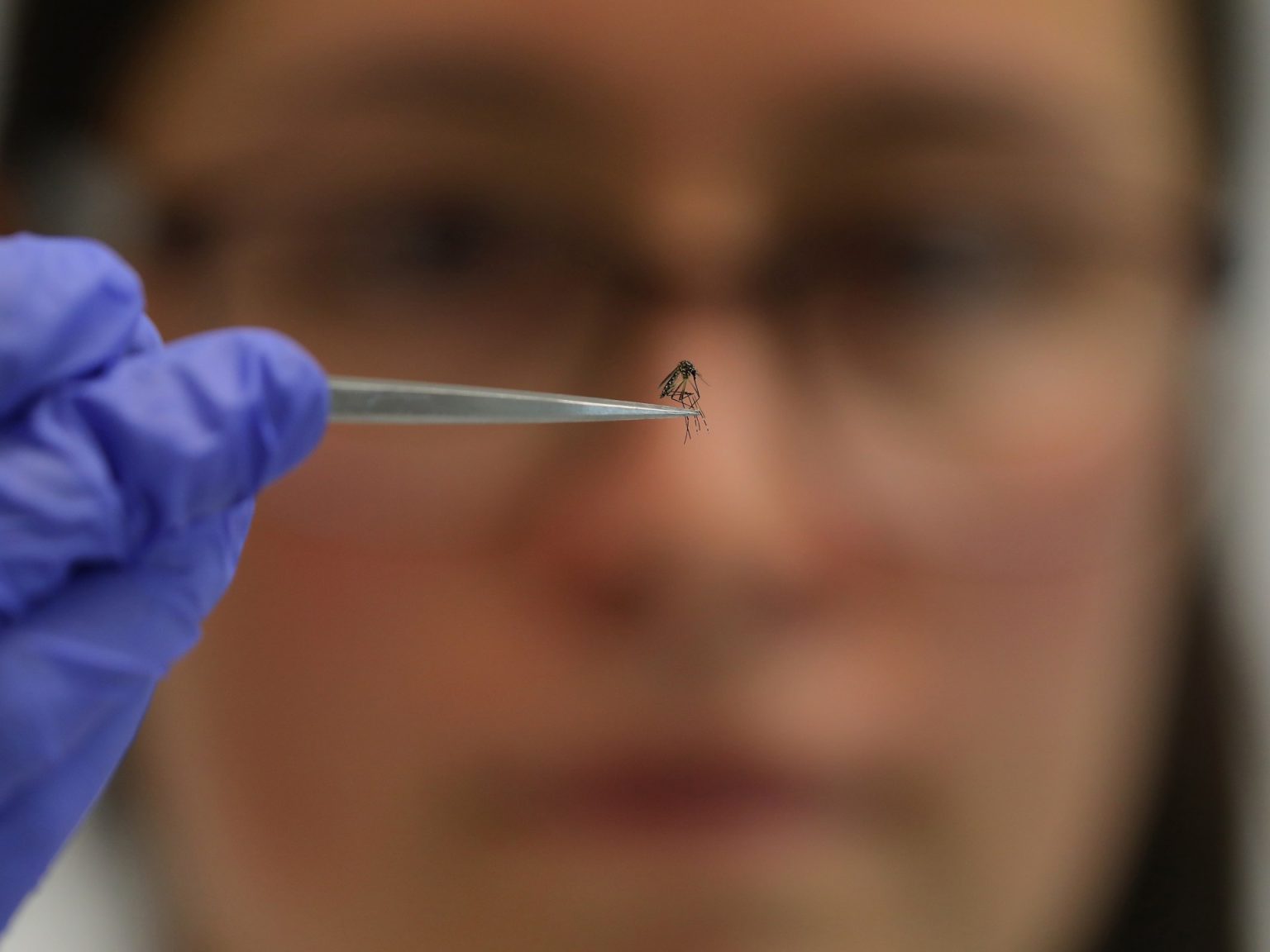
The researchers conducted two clinical trials to evaluate the efficacy of their mosquito-delivered vaccine. The first trial, employing an injectable vaccine derived from a genetically modified parasite (PfSPZ GA1), demonstrated safety but limited efficacy in preventing malaria infection. The second trial focused on two mosquito-delivered vaccines: GA1 and a modified version, GA2. The key difference lay in the duration of liver-stage parasite replication. GA1 replicated for 24 hours, while GA2 replicated for up to a week, providing the immune system with a longer window to recognize and combat the parasite. Participants in the second trial received controlled mosquito bites from mosquitoes carrying either GA1 or GA2, as well as bites from non-infected mosquitoes. A control group received a placebo. Subsequently, all participants were exposed to bites from mosquitoes carrying the unmodified malaria parasite to assess the efficacy of the vaccines.
The results of the second trial revealed a striking disparity between the two vaccine candidates. While only 13% of the GA1 group developed immunity, a remarkable 89% of the GA2 group achieved protection against malaria. The placebo group, predictably, showed no immunity. This stark contrast highlighted the importance of prolonged liver-stage parasite replication in eliciting a protective immune response. The extended exposure afforded by GA2 allowed the immune system ample time to identify and mount a robust defense against the parasite.
Despite the promising results, the small sample size of the second trial (20 participants) necessitates further research to validate the efficacy of the GA2 vaccine. Larger-scale studies are crucial to confirm the observed protection rates and to assess the vaccine’s long-term efficacy against different P. falciparum strains prevalent in malaria-endemic regions. Moreover, the practicalities of deploying mosquito-delivered vaccines on a large scale remain a challenge. While effective in a controlled clinical trial setting, using mosquitoes for mass vaccination is logistically impractical. Therefore, the researchers envision developing a vialled version of the GA2 vaccine for widespread distribution, particularly in Africa, the continent bearing the heaviest burden of malaria.
The concept of using insects as vaccine delivery vehicles is not entirely new. In 2010, Japanese researchers engineered mosquitoes to carry a vaccine against leishmaniasis, another parasitic disease. Rodents bitten by these modified mosquitoes developed antibodies against the leishmaniasis parasite, though the protective efficacy of this approach remains to be fully determined. Similarly, a 2022 study in the United States explored the potential of mosquito-delivered malaria vaccines using CRISPR gene-editing technology. This trial, while showing a 50% efficacy rate, further substantiated the feasibility of using mosquitoes as vaccine vectors.
The development of a mosquito-delivered malaria vaccine represents a paradigm shift in vaccine research. By leveraging the mosquito’s natural transmission mechanism, scientists have devised a potentially transformative approach to combating malaria, a disease that continues to claim hundreds of thousands of lives annually, predominantly in Africa. While further research and development are necessary, this innovative strategy holds immense promise for enhancing malaria control efforts and ultimately eliminating this devastating disease. The transition from mosquito-delivered vaccine in clinical trials to a readily deployable vialled vaccine will be critical for realizing the full potential of this groundbreaking approach.