Norovirus, a common and highly contagious stomach bug, is experiencing a surge in cases across parts of the United States this winter, exceeding typical seasonal trends. The Centers for Disease Control and Prevention (CDC) reported 91 norovirus outbreaks during the week of December 5th, 2023, a substantial increase from the 69 outbreaks reported the previous week and significantly higher than the historical maximum of 65 outbreaks typically observed during that period. This rise in norovirus activity raises concerns about the potential for widespread illness and highlights the importance of preventative measures.
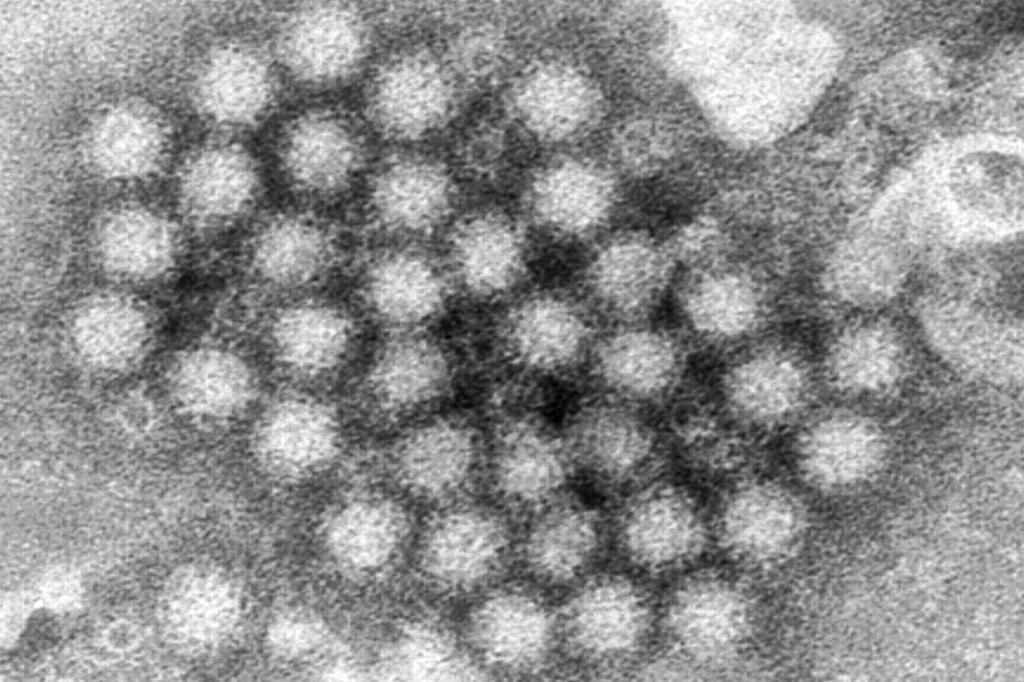
Norovirus, often dubbed the “winter vomiting bug,” is the primary culprit behind foodborne illnesses in the United States. The CDC estimates that norovirus accounts for 58% of all domestically acquired foodborne infections annually. The virus’s remarkable contagiousness stems from its ability to cause illness with an incredibly small infectious dose; as few as 10 viral particles can be enough to trigger an infection. Although norovirus outbreaks can occur year-round, they are most prevalent during the colder months, from November to April, coinciding with increased indoor gatherings and close proximity, facilitating viral transmission.
The hallmark symptoms of a norovirus infection include sudden onset of vomiting and diarrhea, often accompanied by nausea, stomach pain, body aches, headache, and fever. While these symptoms are generally unpleasant, they are typically short-lived, lasting between one and three days for most individuals. However, the virus’s widespread impact is significant. In the United States, norovirus is responsible for an estimated 19 to 21 million illnesses annually, resulting in an average of 900 deaths and 109,000 hospitalizations, predominantly among adults aged 65 and older. Additionally, norovirus infections lead to approximately 465,000 emergency department visits, mostly involving young children.
Norovirus transmission occurs primarily through direct contact with infected individuals, contaminated food or water, or contact with contaminated surfaces. Outbreaks are common in settings where people are in close quarters, such as cruise ships, nursing homes, schools, and correctional facilities. The virus spreads easily through shared food, utensils, and surfaces, highlighting the importance of meticulous hygiene practices. Despite the virus’s prevalence and impact, there is currently no specific antiviral medication to treat norovirus infections. Treatment focuses on managing symptoms and preventing dehydration, a serious complication, especially in vulnerable populations.
Dehydration, arising from persistent vomiting and diarrhea, poses the most significant risk associated with norovirus infection, particularly for young children, older adults, and individuals with weakened immune systems. These vulnerable groups are more susceptible to severe dehydration, potentially requiring hospitalization. Recognizing the signs of dehydration is crucial. Symptoms include decreased urination, dry mouth and throat, and dizziness upon standing. In children, dehydration may manifest as unusual sleepiness, fussiness, or crying with few or no tears. If dehydration is suspected, seeking immediate medical attention is essential.
Protecting oneself and others from norovirus infection hinges on diligent hygiene practices, primarily rigorous handwashing. Washing hands thoroughly with soap and warm water for at least 20 seconds, especially before meals and after using the restroom, is paramount. Regularly disinfecting frequently touched surfaces with household disinfectants can also help reduce the spread of the virus. Avoiding close contact with infected individuals and refraining from sharing food, drinks, and utensils are additional preventative measures. Staying home when ill and practicing proper food handling techniques further contribute to minimizing the risk of norovirus transmission and protecting public health.