Respiratory Syncytial Virus (RSV) has emerged as a significant public health concern in the United States, alongside the ongoing presence of COVID-19 and influenza. This “tripledemic” of respiratory illnesses poses a substantial challenge to healthcare systems and underscores the importance of continued vigilance and preventive measures. The geographical distribution of RSV reveals varying levels of impact across the country, with some states experiencing significantly higher rates of infection than others. Understanding the nature of RSV, its transmission patterns, and the potential complications, particularly for vulnerable populations, is crucial for effective disease management and public health preparedness.
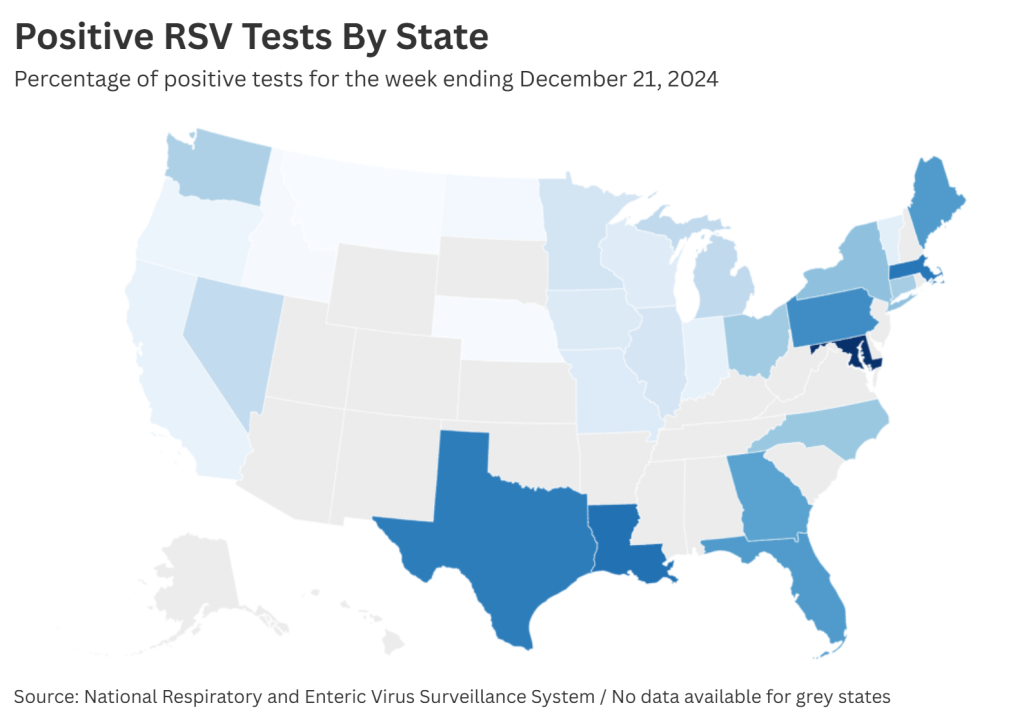
As of the week ending December 21, 2023, data from the Centers for Disease Control and Prevention (CDC) indicated a surge in RSV cases across several states. Louisiana, Massachusetts, and Texas reported the highest percentages of positive RSV tests, ranging from 23% to 25%. Other states, including Pennsylvania, Florida, Georgia, New York, North Carolina, and Ohio, also experienced elevated RSV activity, with positive test rates between 13% and 21%. Conversely, states like Montana, Nebraska, and North Dakota reported significantly lower RSV activity, with positive test rates below 3%. This variation in regional impact highlights the dynamic nature of RSV transmission and underscores the need for tailored public health responses based on local epidemiological data.
RSV, a common respiratory virus, typically causes mild cold-like symptoms in healthy individuals but can pose serious risks to infants, older adults, and those with compromised immune systems. The virus primarily affects the nose, throat, and lungs, making it difficult to distinguish from other respiratory illnesses like the common cold, influenza, and COVID-19 based on symptoms alone. While RSV typically circulates during the late fall and winter months, the 2023 season witnessed an early surge in cases, placing additional strain on healthcare resources. The virus is the leading cause of hospitalization in infants under one year of age, emphasizing the importance of preventive measures and prompt medical attention for this vulnerable population.
The resurgence of RSV, coupled with the ongoing circulation of COVID-19 and influenza, has created a complex public health landscape. The CDC has acknowledged the high levels of respiratory illnesses across the country and anticipates a similar or lower peak in combined hospitalizations from these three viruses compared to the previous year. However, the overall burden of respiratory illnesses remains significantly higher than pre-pandemic levels. This emphasizes the need for continued public health efforts to mitigate the spread of these viruses and protect vulnerable populations. The impact of the COVID-19 pandemic on RSV epidemiology is also a factor. Social distancing measures and mask-wearing adopted during the pandemic likely disrupted the typical transmission patterns of RSV, leading to a susceptible population and contributing to the current surge in cases.
Several factors likely contribute to the current surge in RSV cases. One prominent theory centers on the reduced exposure to common respiratory viruses during the COVID-19 pandemic. Social distancing measures and mask-wearing, while effective in controlling the spread of COVID-19, may have inadvertently limited exposure to other respiratory viruses like RSV. This reduced exposure, particularly among young children, may have created a more susceptible population, contributing to the increased incidence and severity of RSV infections observed in the current season. The return to normal social interactions, including daycare and school attendance, likely further facilitated the spread of RSV among children who had limited prior exposure to the virus.
The CDC continues to actively monitor the evolving situation with respiratory illnesses, including RSV. The agency emphasizes the importance of vaccination against both COVID-19 and influenza as key preventive measures. While an RSV vaccine is not yet universally available, its development and potential rollout are promising developments in the fight against this virus. Continued surveillance and public health messaging regarding hygiene practices, such as frequent handwashing and covering coughs and sneezes, remain crucial in mitigating the spread of RSV and other respiratory illnesses. The experience gained from managing the COVID-19 pandemic has provided valuable insights and tools that can be applied to address the current challenges posed by the resurgence of RSV and other respiratory viruses.