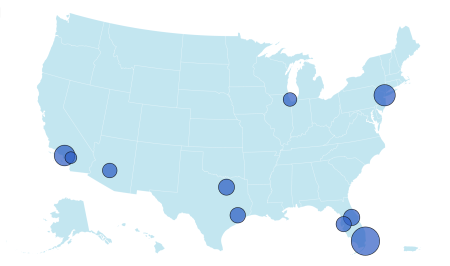
The escalating cost of insulin in the United States has spurred a wave of litigation against major pharmaceutical companies, pharmacy benefit managers (PBMs), and UnitedHealthcare. Dozens of school districts across several states, representing a portion of over 200 districts nationwide, have filed lawsuits in the U.S. District Court for the District of New Jersey, seeking damages and demanding accountability for what they allege is a manipulative scheme to inflate insulin prices. These districts contend that the defendants’ actions constitute fraud and unjust enrichment, forcing them to bear the brunt of exorbitant costs for a life-saving medication essential for their employees and retirees with diabetes. The timing of several lawsuits coincides with the aftermath of a shooting targeting the CEO of UnitedHealthcare, seemingly motivated by anger directed at the health insurance industry and corporate greed, further highlighting the public’s growing frustration with the current healthcare landscape.
At the heart of these lawsuits is the claim that pharmaceutical giants Eli Lilly, Novo Nordisk, and Sanofi, in conjunction with PBMs like CVS Caremark, Express Scripts, and UnitedHealth’s OptumRx, have conspired to artificially inflate insulin prices. The plaintiffs argue that despite declining production costs, the price of insulin has skyrocketed over the past two decades, placing an undue financial burden on health plans. The school districts allege that PBMs, responsible for negotiating drug prices and formulating lists of covered medications (formularies), have exploited their position to extract substantial rebates and fees from manufacturers in exchange for favorable placement on these formularies. These behind-the-scenes financial transactions, concealed from payers like the school districts, have allegedly led to inflated list prices ultimately passed on to health plans, significantly increasing the cost of insulin for consumers.
The plaintiffs point to the stark contrast between the original intent behind insulin’s discovery and its current exorbitant price tag. Insulin, discovered over a century ago, was intended to be an affordable and accessible medication. The patent was sold for a nominal fee to ensure widespread availability. However, the current reality sees patients facing prices of up to $700 per vial, a dramatic departure from the drug’s intended affordability and a testament to the alleged price gouging practices being challenged in court. The lawsuits highlight the widening gap between the original vision of accessible healthcare and the current profit-driven system that has made life-saving medication prohibitively expensive for many.
The legal battle extends beyond the pharmaceutical companies and PBMs to include UnitedHealthcare, a major health insurance provider. The lawsuits allege that UnitedHealthcare played a role in the scheme to inflate insulin prices, further contributing to the financial strain on school districts and other payers. The interconnectedness of these entities within the healthcare system underscores the complexity of the issue and the need for comprehensive reform. The allegations against UnitedHealthcare also connect to broader concerns about corporate greed and the prioritization of profits over patient well-being within the health insurance industry.
The FTC is also involved, investigating PBMs for their role in rising insulin prices. However, CVS Health, UnitedHealth Group, and Cigna have countered by suing the FTC, arguing that its case against them is unconstitutional. This legal maneuvering further complicates the landscape and underscores the significant financial and legal stakes involved. The FTC maintains that its pursuit of the case is justified and necessary to protect consumers from unfair practices that artificially inflate drug prices. The clash between the FTC and these major healthcare corporations highlights the ongoing tension between regulatory efforts to control costs and corporate interests seeking to maximize profits.
The ongoing litigation surrounding insulin pricing has sparked a broader debate about drug pricing practices and access to affordable healthcare in the United States. Experts have noted that insulin prices in the U.S. are significantly higher than in other developed nations. While some advocate for price caps on essential medications like insulin, others express concerns about the potential impact on research and development, suggesting alternative approaches such as easing regulatory burdens or allowing over-the-counter access to insulin, similar to policies in Canada. The lawsuits filed by the school districts represent a significant step towards holding pharmaceutical companies and PBMs accountable for their alleged role in creating this crisis, and the outcome of these cases could have far-reaching implications for the future of drug pricing and healthcare accessibility in the United States. The increasing number of lawsuits and the involvement of various stakeholders, including regulatory bodies and advocacy groups, indicate that this issue will continue to be a focal point in the ongoing struggle for affordable and accessible healthcare.